Louise was scheduled for her third round of TACE today but her bloods have continued to drop. Her platelets are 10 000 as we speak. A normal platelet count ranges from 150,000 to 450,000 (platelets per microliter of blood). So her platelets are 140 000 short of where we would like them to be……..
TACE or RCT?
Lou has had two rounds of TACE (Trans-Arterial percutaneous Chemo-Embolisation). She’s scheduled for four.
Leaving for Germany I thought TACE was the same as RCT (Regional Chemotherapy). TACE is definitely a form of RCT but they are administered and managed differently.
I believe the TACE we have done so far has been of benefit. After two rounds (half the liver each round) Lou has had some positive response. Her Pleural Effusion (water in the lungs ) has slowed. Her tumour cell activity has also decreased, which means some aggression has been removed from the liver tumour metastasis. As you know, the metastasis in young triple negative breast cancer patients is angry as all hell.
The decision junction we’re at now is TACE or RCT? While there are several different forms of RCT, the one proposed for Louise is; Isolated Perfusion with chemofiltration.
The big question is; which option/facility/doctor provides Lou with a better chance of taking down the tumours? Unfortunately, not ever being able to know the answer to this question makes for a tough decision.
I’m very mindful of changing treatments halfway through, so I want to leave both doors open until a progress scan provides more data on our current position. We will acquire a liver MRI when her platelets are on their way back up (>100 000), hopefully within a week.
1.) Professor Vogl and Trans-Arterial Chemo-Embolisation(TACE) Of The Liver
Up to 75% of the normal liver tissue is perfused by the portal venous system and only 25% is supplied by arteries. On the contrary, liver tumors are supplied up to 95% by arteries. Hence chemoembolisation of liver arteries lead to development of ischemic necrosis in the tumor region while the remaining normal liver tissue is spared by sufficient perfusion through the portal venous system.
The half-life of a chemotherapeutic agent is increased by hours to weeks through the stoppage of blood supply.
The procedure as I know it: After local anaesthesia, a puncture is made into the femoral artery in the inguinal region. Doing this, a small femoral sheath is usually placed in the artery through which different catheters or guide-wires can be inserted. The abdominal aorta with its various branches is visualised. Then a very small catheter (micro catheter) is passed through the liver artery into the artery supplying the tumour and the chemoembolisation is performed. You’re given pain meds through infusion during the procedure.
The cocktail is usually strong chemo agents. For Louise, for both her rounds, she had 9.88mg of Mitomycin C, 101,96mg Irinotecan, 50,12mg Cisplatin. This is combined with Lipiodol and Spherex, these two ingredients block the blood vessels.
At the end of TACE Louise was placed in observation for about three hours during which possible complications can be diagnosed and treated (which she’s never needed). She also had an MRI before the procedure and a CT after to evaluate the success of the treatment and to rule out a complication.
This technique allows the toxicity to be >80 times a systemic dose.
Side effects:
Most sources I’ve read say TACE has minimal adverse effects with very little stress for the patient. This, unfortunately, hasn’t been the case with Louise. The side effects for Louise have been severe. They include:
- Extreme nausea
- Inability to move/comatose sleep, for well over a week
- Doesn’t eat and barely drinks = dehydration
- Weight loss – up to 5kg’s
- Scrambled brain like she’s extremely drunk, these side effects last for two weeks
- Key Blood results decrease significantly, apart from the usual side effects and danger this has, it also delays the next treatment significantly
- Massive mental hit
The brain issues are likely to get worse with each treatment, based on treatment one and two. Having her mind scrambled for weeks will have a big effect on her motivation and ability to fight.
2.) Professor Aigner and Regional Chemotherapy (RCT) – Isolated Perfusion of The Liver
In the method suggested for Louise, an arterial port catheter is implanted directly into the tumour-supplying vessel during surgery. This enables the tumour to be treated with the chemo agent over three to four days. This is combined with isolated perfusion where the liver is isolated with a catheter system, so the high cytostatic concentration flows through the liver by means of an external pump.
At the same time heat is supplied to the tumour (hyperthermia) and the oxygen content of the blood supplied to the tumour is reduced.
This method is combined with chemofiltration (extracorporeal detoxification which is like dialysis) to remove excessive amounts of chemotherapeutic agents in the systemic circulation. This is done at the completion of the isolated perfusion phase.
This technique also allows the toxicity to be >80 times higher than a systemic dose.
Side Effects:
None of Aigner’s patients experiences the brain issues Lou experienced with TACE and his patients have a much less severe reaction. “95% have few side effects.”
We’re not guaranteed that Lou will have minimal side effects (as his treating team predicts) but I envisage they will be considerably less.
What’s holding us back from making a decision?
- We don’t yet know how effective the two TACE sessions have been
- An MRI will assist with this
- If Lou has had a reduction in tumour size then we should consider continuing the next two rounds with Vogl
- The door with Vogl could close if we go with Aigner
- I will ask Vogl if this is the case
- We would be changing strategies without completing the current prescribed regime
- We don’t know if Aigner’s treatments are as effective as Vogl (It’s something we will never know)
- I think that they are as effective but maybe I just want to believe this so its apples for apples on the positive treatment output….
Another big ingredient in the decision is our desire to change the chemotherapy agent/s for either treatment choice if the first two rounds of TACE haven’t had a positive enough effect on the tumours in Lou’s liver. This is a whole subject in itself……..one that I will try and explain in my next post….

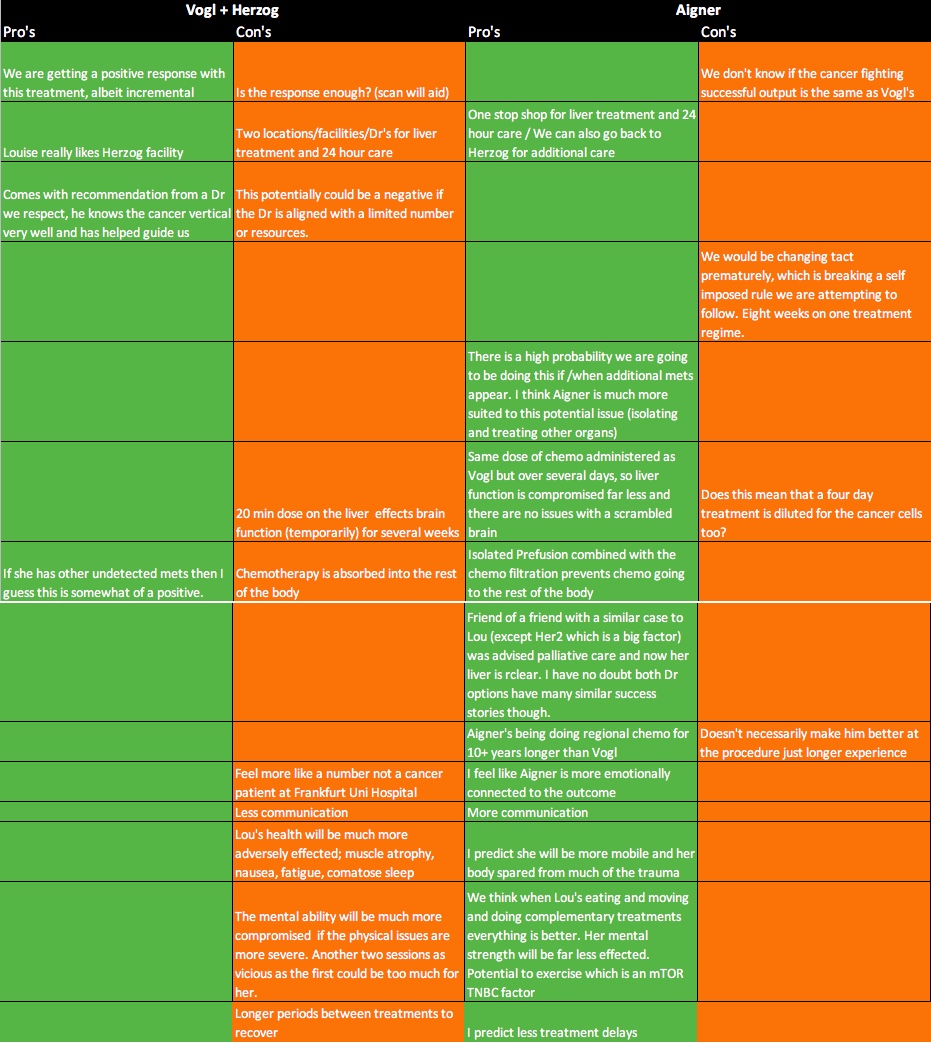
Vogl me thinks
It seems like the positive aspects of Aigner outweigh the negatives of Vogl. From your breakdown it looks to me like a transition would be worthwhile. Sending so much loVe to Lou and you too. xx